Vol. 3, Issue 4 (2017)
Comparative study between DHS and PFN in the management of trochanteric and subtrochanteric femoral fractures
Author(s):
Dr. DV Prasad, Dr. Santusht Kumar, Dr. Yash Rabari, Dr. Neel Bhatt, Dr. Nikhil Suri and Dr. Ajinkya Jadhav
Abstract:
Introduction: The of aim treatment of these fractures is prevention of malunion and early mobilization. There are various treatment options available, the ideal choice of treatment is internal fixation. Most common used device used for fixation is DHS with side plate assemblies. The best suited implant for management is PFN.
Aim and Objectives: (A) Comparative study of PFN AND DHS. (B) Evaluation of effectiveness and strength of PFN and DHS.
Material and methods: The present study was carried out in PRH, Loni from 2016 to 2017.The study consisted of total 40 adult patients of peritrochanteric fractures of femur. Out of this 20 patients were treated with PFN and DHS 20.This was a comparative study. All the peritrochanteric fractures were considered except grade 4 type of intertrochanteric fracture as per Boyd and Griffins classification and grade 5 according to seinsheimer classification. Minimum of 6 months of follow up.
Observation and Result: We have done follow up examination at the end of 6 weeks, 12 weeks, 18 weeks. Average time for which patients were admitted was 3 weeks i.e. 21 days. Average time of union in all our 40 patients was 18 weeks (range 12 to 20 weeks).
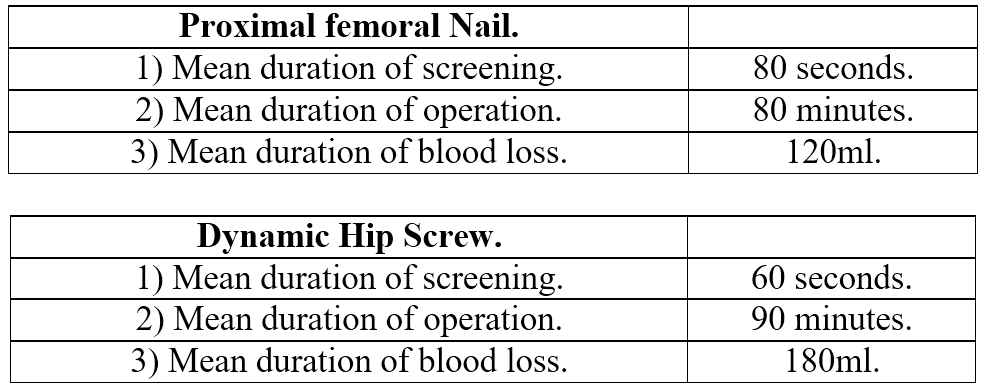
Intraoperative details
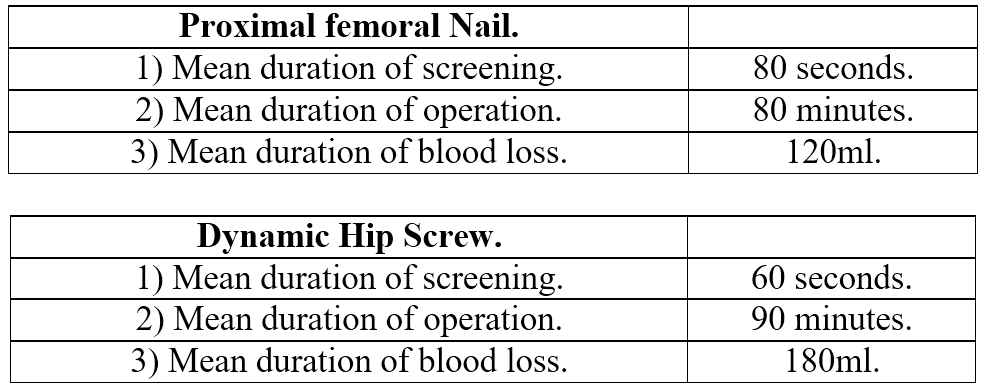
PFN is better treatment modality considering its biomechanical properties. The claimed advantage with PFN is that a smaller exposure is required than for a sliding screw it may therefore be associated with less blood loss, shorter operating time and less morbidity. Also in osteoporotic bone PFN fixation carries definitive advantage over DHS fixation device.
Pages: 106-108 | 3342 Views 501 Downloads
How to cite this article:
Dr. DV Prasad, Dr. Santusht Kumar, Dr. Yash Rabari, Dr. Neel Bhatt, Dr. Nikhil Suri and Dr. Ajinkya Jadhav. Comparative study between DHS and PFN in the management of trochanteric and subtrochanteric femoral fractures. Int. J. Orthop. Sci. 2017;3(4):106-108. DOI: 10.22271/ortho.2017.v3.i4b.17





